![]()
|
THE
HEALTH EPIDEMIC Instead we are inundated with "soft" health information
in the form of regular newsletters from local hospitals, advice columns
in newspapers and on TV and radio, and--increasingly--straight commercials.
I like the one for fiber something-or-other with the guy who starts
out: "I'm not an actor. Just a regular person like you, 30 years
old. But I had a heart attack." He's perfectly deadpan as he advises
us to eat more fiber, especially Brand X cereal. (Later that night,
on the news, "Bran Stocks Soar as Fiber Issues Explode!")
This media bombardment in the form of health advice illustrates two
coexisting but seemingly contradictory trends: on the one hand, the
enormous growth of highly competitive, hi-tech medical industry; on
the other, the tremendous national preoccupation with health maintenance,
a preoccupation partly based on mistrust of the medical industry and
on anxiety about its spiralling costs.
Hospitals: Medical Factories
Hospitals were originally established between about
1880 and 1920. Almost all of these early hospitals were philanthropic
in nature; they were often linked to medical schools in order to provide
students with the "raw material" on which to learn their craft.
Doctors were private practitioners and still had a lot of competition
from "quacks," that is, practitioners of other types of medicine.
After 1945, as antibiotics, new surgical techniques, and other innovations revolutionized western medicine, hospitals belatedly began to undergo the same process that had overtaken so many other industries--mechanization. Only fifty years ago hospitals were health care "workshops," where acutely ill or severely injured patients were brought to receive last-resort care--usually surgery, or else merely asepsis, anesthesia, food, and rest. The most expensive technology was probably the hand-cranked operating table or the autoclave that sterilized the instruments. Today, hospitals are highly diversified factories for testing, drugging, and operating on patients with a vast range of complaints, many of which were either untreatable or unheard-of a generation ago. The typical hospital continually sprouts new specialized wings, "centers," and clinics, and invests in hundreds of thousands of dollars worth of new diagnostic and surgical equipment every year. Moreover, the care in many hospitals, especially giant chains like Kaiser, has a notoriously assembly-line quality; patients are shuffled from one overworked, harrassed technician, nurse, or intern to the next, like sides of beef in an automated slaughterhouse. So how did this expansion happen? Or, as a Bank of America billboard once asked:
"Wherever did they get the money to buy that?"
As with so much of the so-called private sector, the answer, of course,
is: from Uncle Sam. The federal government has been, and continues to
be, the single most important force behind the expansion of the medical
industry. In 1965, the government created Medicare/Medicaid, which brought
many previously uninsured people into the market for private health
care. "Government spending, which had hitherto been concentrated
in relatively small direct grants to public-health programs and public
hospitals, skyrocketed and was directed to the purchase of care in the
private sector. The programs included unlimited payments to hospitals
for capital expenditures--a blank check for private hospital expansion"
(Himmelstein and Woolhandler, "Medicine as Industry," Monthly
Review, April 1984). This subsidy to hospital corporations and doctors, which had the
political advantage of appearing to respond to the militance of poor
people, totaled $48 billion in 1982, with another $25 billion in tax
exemptions for health insurance and non-profit hospitals. Most tellingly,
studies of private hospitals in Oakland, Berkeley, and Boston found
that every major private hospital received more than 60% of its
revenues from government sources. (Monthly Review, op.cit.)
According to the San Francisco Chronicle, hospitals made profits
averaging 12 to 15 percent on Medicare patients in 1984 and 1985, a
far higher rate of return than before Medicare's cost-control payment
system began a year earlier.
Medicine, Capitalism, and the Rate of Exploitation
Medicine's most important function in capitalism was
originally to improve and maintain the working abilities of the population.*
Medical services were "wage goods" that workers paid for--when
they could--out of their own pockets, or else received as charity. (The
knowledge that one generally gets what one pays for helps to explain
the extreme dread of illness, and especially of hospitals, among older
working-class people. A few visits to the doctor were--and still are,
for the uninsured--a severe strain on the budget, and the hospital meant
probable death.) Medicine as a commodity was provided by self-employed
artisans (doctors) rather than by full-scale capitalist enterprises.
As the government subsidized medicine's tremendous expansion, however,
it became a great absorber of capital, growing ever larger and more
influential. Now other capitalists and the government have revolted
and are beginning to insist that medical capital appropriate its share
from individual consumers rather than from individual productive capitalist
firms, from the parasitic but powerful insurance sector, or from the
collective capitalist represented by the government. The method for this transference has been to increase employee payment
shares of company-sponsored health insurance. ("91% of all corporate
employees are insured through company health-insurance plans" (Regina
Herzlinger, "Corporate America's Mission Impossible: Containing
Health Care Costs" in Technology Review, Nov.-Dec.1985.).
In collective bargaining around the country throughout the decade, wage
freezes and rollbacks have not been uncommon, but almost all union contracts
have increased employee contributions to medical coverage. Health insurance
premiums have doubled from the approximately $75 billion spent in 1980.
"The favorite cost-control strategy of many firms has been to
modify health insurance policies. In 1980, for instance, only 5% of
the firms' employees paid a deductible of more than $100 before insurance
payments could begin. By 1984, 43% paid such a deductible..." Similarly,
"in 1980 53% of employees paid nothing for health insurance, but
by 1984 that number had dropped to 38%" (Technology Review,
op.cit.). Cutbacks in maximum coverage and services funded have also
been widespread in the 80s. We can assume that these trends have continued
since 1984.
There is an ironic element to this analysis of the
function of medicine: while it's true that at the level of capitalist
society as a whole, medicine's primary function is to ensure the health
of workers, the U.S. puts relatively little wealth into occupational
health and safety, disability, and retraining. According to a March
1, 1987 NBC News special report, massive falsification of occupational
accident reports is the norm throughout U.S. industry. These reports
are the raw data used by OSHA to determine where problems are and where
to inspect, and to gauge the relative safety of U.S. workplaces--and
OSHA itself is being gutted. This is in keeping with the current trend
away from any kind of long-term economic planning or social engineering
and toward maximum short-term gain, otherwise known as corporate feeding
frenzy. (See Dan Berman, Death on the Job, Monthly Review Press,
for extensive documentation of these trends.)
Such changes are part of a drastic increase in the society-wide rate
of exploitation--that is, the ratio between gross national profit and
the cost of maintaining the workforce as a whole, including the unemployed
and the "unproductive" such as housewives and children. Cutbacks
in government programs for poor people (the "socialized" part
of the total cost of maintaining the U.S. workforce) are widely publicized;
however, "middle-class" workers have been experiencing the
same process, first as wage freezes and cutbacks, and second, as increased
health costs. According to Ivan Illich in his brilliant Medical Nemesis,
before 1950 it took less than a month's income to purchase a year's
worth of medical services, but by the mid-70s this price had risen to
5-7 weeks' income on average. It must be well over two months' worth
per year by now. Furthermore, an ever-increasing proportion of medical industry activity
is billing, marketing, recording, paying, and administrative overhead,
said to amount to some $78 billion in waste in U.S. health care system
annually. "[Part of the problem is that more competition will mean
more such waste. Only competing caregivers require strategic planning,
marketing and pricing overheads. Enduring mistrust between payers and
caregivers multiplies record keeping for each" (Alan Sager, "Opiate
of the Managers" Society, July-Aug. 86). We are witnessing a free-for-all in the medical marketplace, in which
shrewd doctors are creating ambulatory surgical clinics to take high-profit
outpatient surgery away from much larger hospitals. It is comparable
to an entrepreneur setting up a small factory to make specialty products
that can be sold for a hefty profit, thereby wiping out a much larger
producer who balanced some money-losing or low-profit but socially beneficial
activity with the high-profit activity now taken away. Competition leads
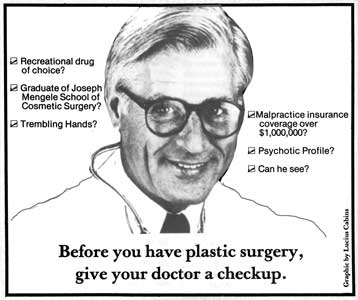
to amputation of unprofitable services from profitable ones. Concentration is bringing in more investment capital, leading to
an increase in for-profit hospitals, ambulatory care centers, and plastic
surgery and other strictly-for-the-rich medical services. It is also
putting the financial squeeze on health workers (see "Kaiser Don't
Care--SEIU Neither" inPW 19). Already, many hospitals are
turning away indigent or uninsured patients, even when they are obviously
in critical condition.
I Have Seen The Future, And it Doesn't Work
Not only is hi-tech commercial medicine engendering
a bloated and unbalanced system of health care, but it is often ineffective
and even dangerous. Illich points out that hospitals have a higher reported
accident rate than any other industry except mining and high-rise construction.
One need not entirely agree with his blistering condemnation of "clinical
iatrogenesis" (in which remedies, physicians, and hospitals are
the pathogens or "sickening agents"--see sidebar) to acknowledge
the growing concern among even mainstream analysts about unnecessary
medical practices running amok. "According to one Harvard medical
school physician, at best only about 30 to 50 percent of health care
services are effective, and the rest border on unnecessary care"
(Technology Review, op.cit.). In fact, there is no national
system of evaluating medical practices. The Food and Drug Administration
oversees, to some extent, the introduction of new chemicals into general
use; but doctors, through the American Medical Association and professional
associations in each state, are left to regulate themselves. They jealously
guard this privilege by intense lobbying and by howling to the media
about "creeping socialism" whenever an upstart legislator
tries to introduce some government oversight. In his Society article, Alan Sager says, "We should cut
clinical costs by identifying what care works and what does not... we
could make rapid progress... if we devote a fraction of the money now
wasted in processing health insurance claims to studying what works"
(Society, op.cit.). Regina Herzlinger makes a similar point in
her Technology Review article: "Files on insurance payments
are massive, but they are organized to facilitate payments rather than
to identify patterns of use."
Health Care Alternatives, Limited
Given that "modern" medical techniques remain
largely unevaluated, it's no surprise that alternative health care has
attracted many people. Since my early adulthood in the mid-70s, my friends
and acquaintances have been seriously concerned about their health.
They have spent countless hours dutifully exercising and studying nutrition,
self-help health practices, macrobiotics, or yoga. Many have also turned
to acupuncture, chiropractic, homeopathy, and numerous other "health
care options." This pursuit, shared by millions of Americans, may
be partly an attempt to gain control over an out-of-control life. It
is also cheaper and often more effective: you don't need $250,000 machines
to create or administer Chinese herbs, and limiting your intake of saturated
fats is undoubtedly better than bypass surgery. However, I am not concerned
here with the efficacy of any particular alternative therapy or preventive
practice. My intention is, rather, to suggest a paradox: the possible
contribution of such therapies and practices to fueling the demand for
health care in general. The strange fact is that despite the enormous growth in self-care,
the market for medical services has not shrunk. Instead it has grown
by leaps and bounds. By helping to discredit hi-tech medicine, alternative
therapies have aided their own economic cause, undoubtedly benefitting
thousands of people in the process. However, they also have contributed
to a great expansion in the amount of health care that people feel they
need. Moreover, much of the people-before-profits philosophy that informed
the early alternative health care movement was lost in the rush to develop
and offer workable alternatives to hi-tech hospitals. The critique of
health as a commodity, never very well developed, evaporated entirely
as holistic entrepreneurs put up a supermarket of alternative therapies.
Many became rich in the process. The range of choices in this therapeutic supermarket is directly
affected by insurance companies' willingness to fund specific treatments.
As alternative health options have gained in popularity, medical insurance
has branched out to provide limited coverage for acupuncture, homeopathy,
chiropractic, and so forth. Insurers recognize that any medical
therapy, regardless of actual efficacy, is a source of profit as long
as premiums stay ahead of insurance benefit payments. Others who are profiting from the health boom include manufacturers
of vitamins and other dietary supplements, suppliers of exercise clothes
and equipment, and makers of "natural" foods. Meanwhile, as
usual in this society, form has overwhelmed substance. Factory-farm
eggs tinted brown to simulate the free-range product of yore are sold
in every supermarket, and even sugar-laden granola bars are now marketed
as health products. There is no evidence, moreover, that the consumers
of all these "healthy" products are any less likely to head
for the nearest clinic or hospital when something goes seriously wrong.
This may be partly because the health-care industry has also exploited wellness ideology with great success. The critique of hi-tech hospitals pre-dates by more than a decade the current attempts to curb hospital economic growth. Alternativists of the 60s correctly argued against the unlimited application of drugs and machines to treat disease. But as their medical "less-is-more" message seeped through the general population, it also blended nicely with the medical industry's need to cut costs and diversify.
Astute health care corporations are de-emphasizing capital-intensive
diagnostic and curative services in favor of "health maintenance"
centers and clinics for every conceivable subgroup of the population--pregnant
mothers, nursing mothers, women in general, infants, children, older
people, athletes--and for various parts of the body--the breast, the
foot, the back, and so on. How long before we see the Midlife Woman
Executive's Toe Clinic, or the Sporting Father's Elbow Center? And how
much illness or injury do such centers and clinics really prevent? True,
some cancers and other problems are best caught early, but the preventive
care mystique is clearly being exploited by the medical industry in
order to keep healthy people passing through its doors. The alternative health movement has ended up reinforcing the system
it set out to transform. Its objections to orthodox, drug-and-machine
medicine have both provided an ideological cover for shifting health
care costs back onto workers and opened up new markets in corporate-style
preventive care. More profoundly, the failure of the alternative health
care movement to develop and popularize an analysis of the social
causes and treatment of illness has fed into the continuing substitution
of paid services for human community.
The Social Psychology of the Service Economy
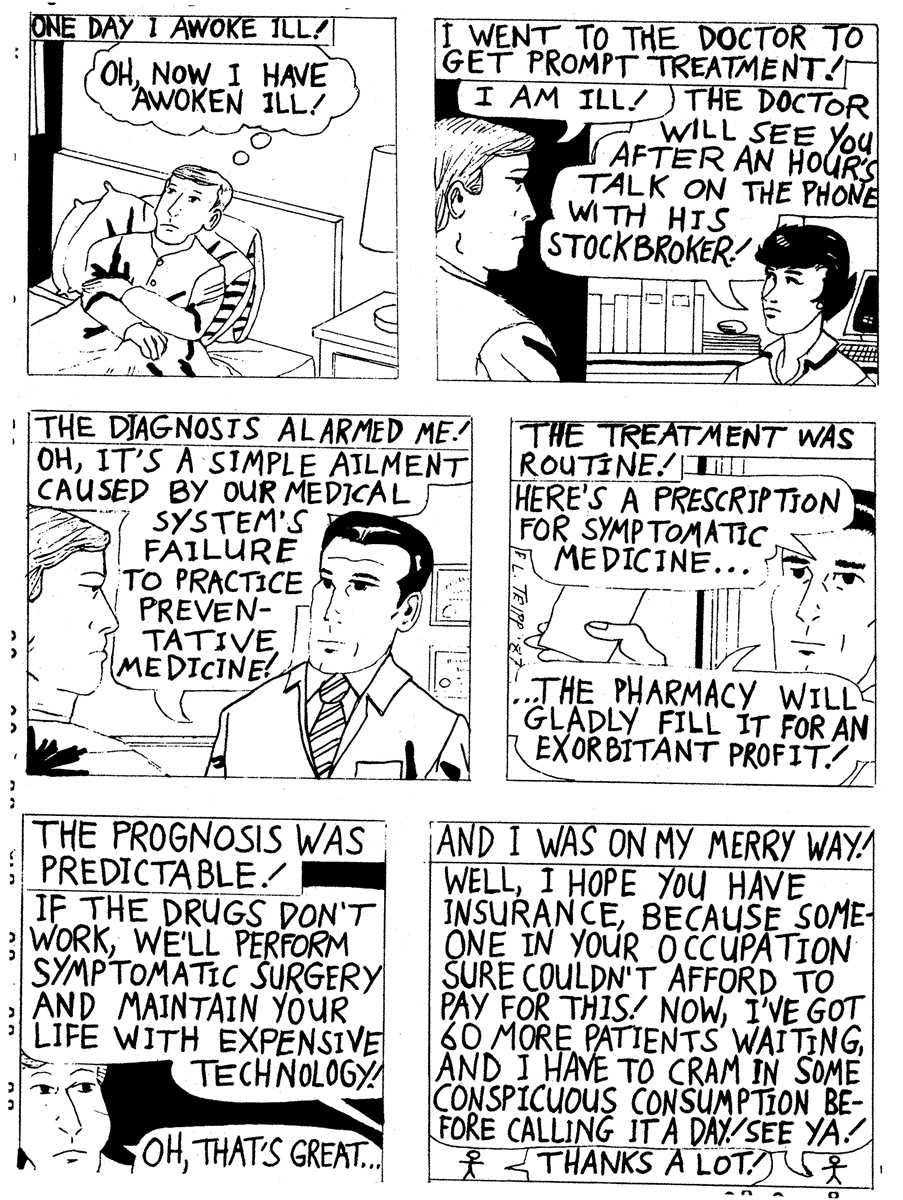
In the simple act of going to the doctor, people reproduce
an elaborate and ideologically loaded set of social relations: The patient
has an illness. The doctor, the expert, will define the
illness by objectively examining and testing the patient's
body. The patient or her insurer will pay for this
service. The doctor will then treat the patient's illness, often
by prescribing drugs manufactured by pharmaceutical companies
that the patient must buy from another expert called a pharmacist.
These roles, actions, and definitions are not "natural." Calling
them into question provides a window onto the psychological and structural
transformations that have accompanied the rise of the service economy. This rise has meant that more and more of the things people once
did for themselves are now being sold to them by corporations or independent
professionals. Health care is among the most glaring examples. Today,
most people have abandoned home remedies for over-the-counter drugs
and/or a visit to the doctor, who often authorizes prescription drugs.
If the doctor runs tests, diagnostic machines get used, thus helping
to pay their amortization cost. And behind the doctor and the clinic
or hospital she probably works for stand the multinational pharmaceutical
companies, the "med-tech" equipment builders, the genetic
engineering firms... It's a classic example of the Invasion of the Marketplace. As the service economy pushes its frontiers outward with the shock
troops of advertising, most people come to see their problems as individual
predicaments to be solved by purchasing the right product or service.
They have less and less confidence that they can solve their problems
themselves or with the help of friends or family. This lack of confidence
in turn legitimates the expertise of the professional who provides the
purchased service. Lack of confidence, moreover, is exacerbated by lack
of time, as long commutes and unpaid "salaried" overtime further
eat up the day, and by lack of human support, as atomized suburbs and
rootless, neighborless urban "neighborhoods" isolate their
residents. More and more areas of human endeavor and interaction are falling
under the sway of the marketplace. A commonly cited example is the ever-growing
use of the courts--and therefore of lawyers--to settle disputes that
would once have been settled by community mediation, or perhaps by a
fist-fight. Likewise, professional "counseling" or low-intensity
psychotherapy now often substitutes for talking your problems over with
a close friend. Other common species are the home computer consultant,
the travel agent, and the resume expert. Not that such professionals
don't often offer useful and time-saving services; I have benefitted
from them myself. My point here is the way our rushed, anxious, and
isolated existence makes us increasingly dependent on them. Even the
lowest-paid workers buy the services of fast food franchises and child
care centers as well as those of the omnipresent lawyers and doctors.
Social Change As Public Health
Ironically, most of the great victories over infectious
disease resulted from improvements in public health rather than from
the treatment of individuals. The creation of underground sewer and
piped water systems, along with slum clearance, played important roles
in this process; however, the decisive factor seems to have been the
strengthening of immune systems owing to better diet (see
sidebar). That better diet was paid for out of higher wages. And where did
these higher wages come from? Certainly not from the humanitarian pleading
of the medical profession, still less from the willing beneficence of
the business class. They were won by the dogged efforts of countless,
anonymous working men and women, who, in the course of countless strikes,
picketed, sabotaged, occupied, dynamited, and otherwise made the lives
of their employers uncomfortable and unprofitable until their demands
were met. These men and women knew perfectly well that their health
and that of their families was not a personal problem; they knew that
lack of fresh produce translated into constant colds and influenza,
lack of milk into rickets and thin hair, bad water into dysentery and
cholera, and twelve-hour workdays under hazardous conditions into short,
exhausted, hopeless lives. Throughout Asia, Africa, and Latin America,
these battles are still being fought; and even here, the gains of the
last half century are endangered.* Meanwhile, other fronts have opened
up.
* If any further evidence were needed, a recent study,
cited in the 8/7/87 San Francisco Examiner, concludes that about
half of all patients admitted to intensive care in U.S. hospitals are
suffering from malnutrition, and that doctors seldom recognize malnutrition
when they see it because it has been omitted from their training.
The most obvious of these fronts is environmental
pollution. The well-publicized disasters like Love Canal, the Rhine,
Bhopal, or Chernobyl, horrific as they are, are only the surface of
the problem. In their normal operation, the chemical plants and nuclear
reactors of the world are Bhopals and Chernobyls in slow motion, releasing
legal, "permissible" levels of radioactivity and chemotoxins
that are accumulating in the biosphere, climbing the food chain toward
us, or settling into our lungs, our fatty tissue, and our bones. Another front is the conditions of work in the new "clean"
sectors, including the health-care industry itself. Processed
World has helped to publicize the health risks facing VDT operators,
telephone service reps, and chip makers. The stress and the poisons
associated with these jobs are combining with other environmental toxins
in an unpredictably hideous synergy to produce cancer, infertility,
miscarriages and birth defects, and various kinds of immune deficiency.
Just as the well-to-do in the last century blamed the bad health
of impoverished workers on their laziness and insanitary habits, business,
government, and the mass media routinely ignore or suppress the connections
between polluted environment and hazardous work on the one hand and
new kinds of illness on the other. And this silence and silencing still
goes largely unchallenged. Interior Secretary Donald Hodel didn't actually
get away with suggesting that we step out in sunscreen, dark glasses,
and long sleeves as a substitute for halting the destruction of the
ozone layer by refrigerants; but he obviously thought he was going to.
The health care industry depends on a sustained demand for its services
just like any other. Is it surprising, then, that there is a tremendous
institutionalized resistance to accepting the powerful arguments linking
disease to environmental and occupational causes? No matter how sound
the ethics of many individual physicians or health bureaucrats, the
health care industry needs continuing high levels of sickness.
Attributing illness to individual behavior accomplishes at least two
things: 1) It ensures ongoing sources of demand, that is, it reinforces
people's acceptance of environmental sickening agents. 2) Sick or hurt people are disempowered and less likely to see themselves as part of a larger group; the lingering suspicion is that some mistake or moral failing caused their illnesses or accidents. This prejudice is particularly obvious in the case of that great killer, the car accident. The social choice to kill some 10,000 people a year by maintaining a transit system based on private autos is passed off as the victims' "bad driving" or "bad luck." Unfortunately, the holistic health movement's justified insistence
on the close connections between mind and body--specifically, between
brain chemistry and the immune system--has also fed into this ideology.
Cancer victims, for instance, are often suspected of having had a bad
diet or some sort of neurosis. This leads, pathetically, to the faith
that "looking after ourselves" will prevent such catastrophes,
and to blaming ourselves when it does not. I am haunted by a scene in
Unnatural Causes, a recent network docudrama about Agent Orange:
a Vietnam vet who was massively exposed to dioxin ten years earlier
is told that he has multiple inoperable tumors. "But I don't smoke,
I eat all natural foods and stuff," he stammers. "It's not
fair." In Europe after World War II, working-class demands for a collective
solution to health problems forced the creation of national health services
that dispensed medical care at low or no cost to all citizens, and (in
Britain at least) emphasized preventive care. These services persist
to this day, despite the efforts of recent right-wing governments to
abolish them. National health insurance is a favorite plank in the platforms
of liberal Democrats, and it is still not a bad goal. It would, however,
leave untouched the broader public health problems I have alluded to.
It is not merely health care that should be a human right, but
freedom from socially and technologically created pathogens--from hunger
to excessive stress, from cotton dust to PCBs. The struggle for health
now is the struggle to transform the entire structure of our society. Lest this seem overwhelming, there are plenty of places to start.
What might happen, for instance, if community groups fighting a hospital
expansion went beyond questions of land use and "environmental
impact" to assert their right to evaluate the medical philosophy,
efforts, and expenditures of the hospital? The same principle
could and should be applied to factories, office buildings, and other
workplaces. Other more conventional kinds of biological self-defense,
like fighting against nuclear power and toxic waste dumping, and for
safer, more relaxed working conditions, are all essential too. Such
health insurance as we have needs expanding. More anti-AIDS funds must
be squeezed out of the government. All these campaigns might be waged
more effectively, however, if the participants situated them within
a long-term struggle for collective, democratic control over all aspects
of social life, and for a sane relationship to the biosphere. In the
final analysis, our health is the health of the planet, and both depend
on our creating a vastly freer and more cooperative world. We don't
have forever.
by Lucius Cabins & Louis
Michaelson
|
|
 |
|
 |
|
|
PATIENTS
AS PRODUCT LINES
The privatization
of publicly funded (through Medicare, Medicaid, and Blue Cross and other
"voluntary" insurance programs) health care may turn out to
be one of the most socially damaging legacies of the Reagan administration.
It has forced hospitals to be run as profit making institutions with
one eye on the product line (in this case, patient care) and the other
on the bottom line. In that halcyon
year of voodoo economics, 1982, the State of California decided to control
rising health costs by making hospitals more competitive. To this end,
it passed legislation that required hospitals to bid competitively for
the privilege of being MediCal (the state's insurance plan for the medically
indigent) providers. The bidding was on a per diem rate with collateral
costs, such as x-rays and lab tests, averaged in. Only those hospitals
whose bids were within the state's guidelines would receive MediCal
reimbursement. This legislation
also allowed insurance companies to offer Preferred Provider Organization
(PPO) contracts. Under the PPO system, a hospital agrees to charge the
insurance company a special rate for its clients. In return, the insurance
company more-or-less guarantees a certain volume of patients to its
preferred hospitals. It does this by charging insurees a larger proportion
of the hospital bill, if they choose a non-PPO facility. For the hospitals,
the new economics meant a change in the way they do business. Before
a hospital cuts a deal with an insurance company, it must figure how
much it costs to treat certain groups of patients (coronary bypass,
maternity, trauma, etc.) and how much it can charge and still remain
competitive. What the insurer is later billed depends on the predetermined
amount assigned to each diagnostic group irrespective of the actual
cost of a particular patient's treatment. Simply put, the hospital receives
the same amount for treating a broken leg whether three x-rays are taken
or four. Since some diagnostic
groups--or product lines--are more profitable for a hospital than others,
hospitals try to make deals with those insurers whose clients needs
are most compatible with their optimum "case-mix". (A case-mix
is the per cent of patients in each diagnostic group a hospital treats.)
Hospitals, like any manufacturing or retail operation, must provide
a range of goods and services with the more profitable business lines
financing other less profitable, but still necessary, activity. The
ideal case mix varies from hospital to hospital, like the ideal product
mix varies from store to store. (Some lines--like burn units or furniture--use
up so many resources that they are rarely profitable, while others--like
birth centers and sportswear--are proven moneymakers.) If, for example,
a hospital makes more money on coronary care than trauma cases, it may
decide not to do business with an insurer who has a lot of young people
on its books who are more likely to be in car or sports-related accidents. Still, hospitals can not
always pick and choose their patients. If a patient's costs run over
what the insurer has agreed to pay, the treatment comes out of the hospital's
profits. There have been published complaints from doctors and nurses
who feel that patients may be discharged too early because of pressures
from hospital administrators to cut costs. Perhaps, the threat of a
malpractice suit is the patient's only defense against cut-rate treatment.
Meanwhile, hospitals spend huge sums on public relations and advertising
in order to fill their beds. The situation is not unlike a restaurant
that would rather serve three parties at a table during the dinner hour
than have one party linger for the whole evening. As they rush the first
group of diners out the door, they are busy scouting for new customers. The PPO system
works, but probably not in the way it was intended. Hospital and insurance
costs have not gone down, but the hospital industry is thriving judging
from the expansion of existing facilities and the increasing number
of for-profit institutions like the Humana group. As it was explained
to me when I interviewed for a job in the data processing department
of St. Mary's hospital in Daly City, even not-for-profit hospitals run
by nuns have to act like profit making corporations in order to survive. If health care can be privatized,
why not the educational system through the use
of school vouchers, as some have proposed?
(I can imagine schools contracting to teach the 3 Rs to students
they considered teachable, with the rest being consigned to the educational
equivalent of the county hospital.)
The public schools are a disaster, not because they are supported
by the state, but because they are so poorly supported; still most people
would not want to see education put entirely into private hands. Isn't
medical care analogous to education? Finally, the question is do we want the quality
of our hospital care to be influenced by some corporation's bottom line? by
Ana Logue |
|
|
MIRACULOUS
MEDICINE?
excerpted
from MEDICAL NEMESIS by Ivan Illich, Bantam paperback,
p. 5 Dorland's Illustrated
Medical Dictionary
25th ed. (Philadelphia: Saunders, 1974):
"Iatrogenic (iatro--Gr. physician, gennam--Gr.
to produce). Resulting from the activity of physicians. Originally applied to disorders induced in
the patient by autosuggestion based on the physician's examination manner,
or discussion, the term is now applied to any adverse condition in a
patient occurring as the result of treatment by a physician or surgeon." "The study
of the evolution of disease patterns provides evidence that during the
last century doctors have affected epidemics no more profoundly than
did priests during earlier times. Epidemics came and went, imprecated by both but touched by neither.
They are not modified any more decisively by the rituals performed
in medical clinics than by the those customary at religious shrines...
The infections
that prevailed at the outset of the industrial age illustrate how medicine
came by its reputation. Tuberculosis, for instance, reached a peak over two generations.
In New York in 1812, the death rate was estimated to be higher
than 700 per 10,000; by 1882, when Koch first isolated and cultured
the bacillus, it had already declined to 370 per 10,000.
The rate was down to 180 when the first sanitorium was opened
in 1910, even though "consumption' still held second place in the
mortality tables. After World
War II, but before antibiotics became routine, it had slipped into eleventh
place with a rate of 48. Cholera,
dysentery, and typhoid similarly peaked and dwindled outside the physician's
control. By the time their etiology
was understood and their therapy had become specific, these diseases
had lost much of their virulence and hence their social importance.
The combined death rate from scarlet fever, diphtheria, whooping
cough, and measles among children up to fifteen shows that nearly 90
percent of the total decline in mortality between 1860 and 1965 had
occurred before the introduction of antibiotics and widespread immunization.
In part this recession may be attributed to improved housing
and to a decrease in the virulence of micro-organisms, but by far the
most important factor was a higher host-resistance due to better nutrition...
Two things are certain: the professional practice of physicians cannot
be credited with the elimination of old forms of mortality or morbidity,
nor should it be blamed for the increased expectancy of life spent in
suffering from the new diseases. For more than a century, analysis of disease
trends has shown that the environment is the primary determinant of
the state of general health of any population."(Emphasis added) |